In earlier parts of this series, I discussed what happens when your body is exposed to extreme cold, a condition known as hypothermia. Left untreated, general hypothermia leads to failure of various organ systems and even death. Besides general hypothermia, however, there are local cold-related injuries, such as frostbite and immersion foot.
What Causes Frostbite?

The body responds to cold temperatures by narrowing the blood vessels, something called “vasoconstriction.” Blood flow to the extremities decreases to preserve flow to the vital internal organs in the body core. As the blood is redirected away from hands and feet, these parts of the body get colder, and ice crystals can form and destroy tissue.
Stages of Frostbite
Frostbite usually occurs in the extremities, but sometimes affects areas like the ears and nose. It occurs in stages that cause more and more damage as time goes on.
First stage: Frostnip- In frostnip, the skin turns red and cold and the victim experiences pain, numbness, and a “pins and needles” sensation.
Second stage: Superficial Frostbite- This causes skin to lose color, going from red to white to blue. At this point, tissues are freezing and swelling may be noted. The texture of the skin changes too, becoming stiff and waxy. Although frozen the victim may feel the sensation of “heat” in the area affected.
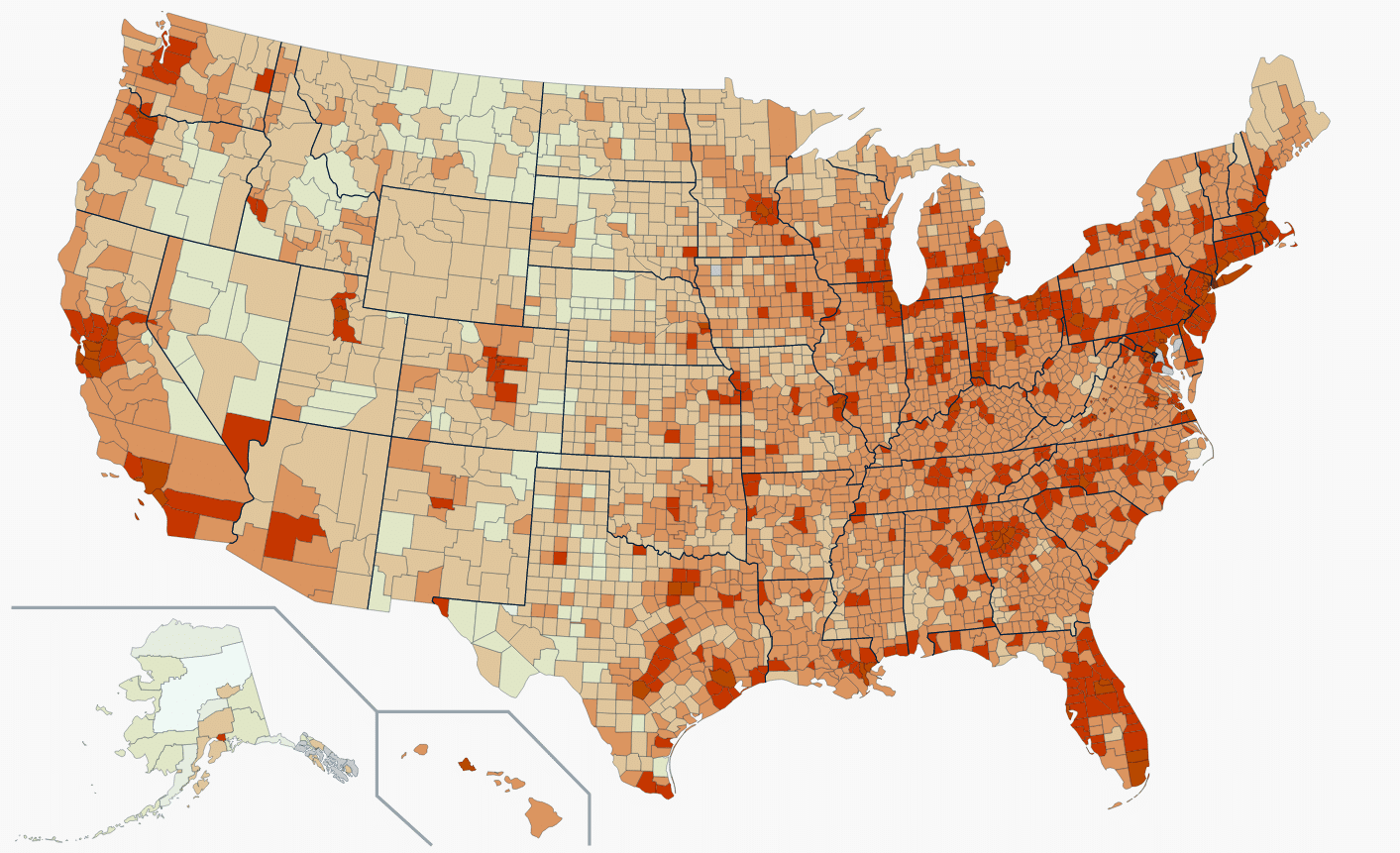
 Gangrene
Gangrene
Frostbite- In third-stage frostbite, both superficial and deep tissues are affected. The skin appears blue and splotchy and circulation is blocked by clotting blood. Even after rewarming, many will develop dark, blood-filled blisters within the first 24-48 hours. Loss of sensation and malfunction of nearby muscles are common consequences.
Although rewarming is appropriate, it may not succeed in deep frostbite cases. An ominous sign is when tissue turns black, a condition known as “gangrene.” Gangrene is the death of tissue resulting from loss of circulation. Once this happens, amputation may be required to remove non-viable parts before infection sets in.
Immersion Foot/Trench Foot
A condition related to frostbite is “immersion foot.” Once known as “trench foot,” this condition was seen commonly in soldiers who spent long periods of time in cold and waterlogged trenches during World War I. Immersion foot doesn’t freeze tissue solid, but causes damage to nerves and small blood vessels due to prolonged time in water 60 degrees Fahrenheit or lower. Immersion foot is a non-freezing injury that appears like frostbite, but might have a more swollen, wet appearance.
Treating Cold-Related Injuries

Rewarming a frostbite injury can be painful but should begin as soon as possible in survival settings to avoid further trauma and improve the chances of full recovery. Most use warm water soaks (no more than 103-4 degrees F or 39 degrees C) on the affected extremity for 30 minutes or until the skin returns to red. The water can’t be so hot that it’s uncomfortable when you place your own hand in it. It should remain warm, however, so replace cooling water as needed. Note that the practice of using warm soaks to treat frostbitten hands and feet is different from that of general hypothermia, which is best treated with warm dry compresses to the groin, neck, and armpits.
In superficial frostbite, clear blisters may form in the damaged area as the patient recovers. In deep frostbite, they’ll likely be filled with blood, and skin may appear bruised, blue, or otherwise discolored. Expect them to turn into thick dark scabs. Some of this tissue may be non-viable and have to be removed. That process is called debridement, discussed elsewhere on this site.
 debridement
debridement
Patients often complain of burning or stinging, which can be treated with ibuprofen at standard dosages (up to 600 mg four times daily). This may or may not help the pain much but will decrease the constriction of blood vessels and decrease further tissue damage. If you can help it, don’t use the frozen extremity for walking, climbing, or other activity.
Although many victims recover completely from superficial frostbite, others have permanent issues with pain or numbness in the affected area. Infection is a possibility and may require antibiotics.
Here’s some other treatment tips:
- Don’t allow thawed tissue to freeze again. The more often tissue freezes, thaws, and re-freezes, the deeper the damage. If you can’t prevent your patient from being exposed to freezing temperatures again, you should wait before rewarming, but not more than a day.
- Don’t rub or massage frostbitten areas. Doing so will result in worse damage to already injured tissue. For the same reason, prevent the victim from walking on frostbitten toes.
- Avoid the use of heat lamps or fires to treat frostbite. The area is numb and can’t feel the frostbitten tissue, sometimes causing significant burns.
There is controversy as to whether frostbitten areas should be bandaged. Some advocate placing absorbent padding between frostbitten toes and fingers. Others suggest leaving it open to air.
Preventing Frostbite

Prevention is hugely important. Wear appropriate clothing that protects your extremities, such as:
- well-insulated boots and a thick pair of well-fitting socks on your feet.
- mittens for your hands; they provide better protection against very cold weather than gloves
- a warm, weatherproof hat that covers your ears – it’s important to protect your head from the cold.
- Add multiple thin layers of warm, loose-fitting clothing which act as insulation. Keep them dry and remove any wet clothing as soon possible.
With some preparation, a cold weather injury doesn’t have to be more than a bump on the road, not the end of the road, for you and your family.
Joe Alton MD

Read the full article here










Leave a Reply